The world has been plagued by the COVID-19 pandemic for more than three years. It has profoundly changed our society, and many people have become generally more fearful. This, in turn, sabotages their immune systems and makes them more vulnerable to COVID-19 infection.
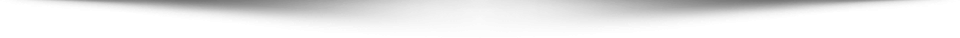
According to a study by a team of researchers from the University of Rochester who examined people’s mental health concerns during the COVID-19 pandemic, fear was the most prevalent issue.
“Fear” was also the most frequently mentioned word on social media, followed by keywords such as “alone,” “failure,” and “depressed.”
Prevalent fears included death, loss of family or friends, vaccine adverse events, COVID-19 infection, and long COVID. For instance, while some people were trying to stay away from COVID-19 vaccines, some were afraid of “missing out” on the most effective brand by choosing the “wrong” ones.
Several other forms of fear include panic and phobia.
Some people were afraid of contracting the virus. As a result, when COVID-19 vaccines became available, they received four to five doses, including booster shots. These people also wore N95 masks and strictly observed social distancing rules. Even with masks, they were fearful of entering a crowd to perform daily duties, such as grocery shopping.
Others were concerned about vaccine side effects and adverse events. They might have elected to get vaccinated as a requirement to stay employed, but they still kept worrying over the potential side effects, such as myocarditis.
These heightened fears may have negatively affected people’s health in many different ways, and fear’s effect on our immune systems can be detrimental.
A Bout of Fear Can Temporarily Boost Our Immunity
Fear, the unpleasant emotion that comes in response to danger, is a necessary bodily mechanism essential to our survival. In the short term, fear can actually boost our immunity.
When we sense that danger is imminent, fear sends our bodies into “fight-or-flight” mode, which equips us with the necessary energy to either flee the danger or prepare for a fight. Fear makes us more vigilant and prompts us to take protective measures that we deem useful in response to a threat like COVID-19.
The immune system also increases its antiviral activity when we perceive a risk of viral infection. The brain’s amygdala will alert the nervous system. The pituitary and adrenal glands will then increase the production of stress hormones, such as cortisol and adrenaline, and circulate them in the blood.
Cortisol is generally anti-inflammatory, and it makes glucose more available to the muscles and brain. Adrenaline, also known as epinephrine, can increase the heart rate and blood pressure, expand the air passages of the lungs, improve vision and other senses, and redistribute more blood to the muscles. Adrenaline can also increase the number of monocytes and neutrophils, both of which are white blood cells, and send them into the bloodstream while sending another type of white blood cell, called lymphocytes, into other tissues.
BY FITNUSBRACE
Why Fear Sabotages Our Immunity
Although a bout of fear can enhance our immunity and boost our chance of survival, being in a constant state of fear for a prolonged period can also create health problems—and weaken the immune system.
Stress Hormones Inhibit Immune Cells
Cortisol and adrenaline, although helpful for short vigilance, are actually stress hormones.
If a person has consistently high levels of cortisol, the body will eventually become used to having an excessive amount of cortisol. According to a study recently published in the journal Brain Sciences, such chronic elevation of cortisol can lead to increased activation of inflammatory cytokines and promote insulin resistance. And the worsened insulin-resistance situation will, in turn, contribute to more inflammation. These incidents can lead to chronic inflammation of the body and a weakened immune system.
Consistently high levels of adrenaline, as well as cortisol induced by fear, can weaken the body’s immune system because of their inhibitory effect on many immune cells. Cortisol is the primary glucocorticoid. Glucocorticoids significantly reduce the number of circulating immune cells, including T cells and macrophages.
In one study published in the journal Brain, Behavior, and Immunity, one group of people who have the trait of worry was exposed to a phobic stimulus, while another group with the same trait wasn’t exposed. The results show that both groups experienced increased heart rate, but the group that was fearful due to the stimulus didn’t have an increase in natural killer cells—a kind of immune cell—in their peripheral blood, while the other group did.
In a study published in the journal Nature, the authors found that the brain’s fear circuit could regulate immune cells during acute stress.
The “fear circuitry” is mainly composed of the amygdala, nucleus accumbens, bed nucleus of stria terminalis, hippocampus, and ventromedial hypothalamus. According to an article published in The Journal of Neuroscience, although fear and anxiety are distinct emotions, they share the same underlying neural circuitry, as fear is a negative emotional response to a certain threat, while anxiety is the response to an uncertain threat.
The researchers of the study published in Nature discovered that during acute stress in mice, different brain regions shaped the distribution of immune cells and the function of the entire body. For instance, the researchers found that acute stress redistributed immune cells from peripheral organs, such as muscles and blood vessels, to the bone marrow, and the number of B cells (important to the adaptive humoral immune system) and T cells in the lymph nodes was also reduced.
Researchers also found that acute stress altered innate immunity by directing neutrophil recruitment to sites of injury.
Fear Affects the Endocrine System and Can Cause Hormone Problems
When fear initiates the fight-or-flight response, the amygdala signals the hypothalamus to activate the pituitary gland, which is considered the “master gland” of the endocrine system, as it also controls many of the other glands. The endocrine system (aka, hormone system) is composed of glands that produce hormones to regulate many bodily processes, including mood, energy level, blood pressure, appetite, and immunity.
Since hormones directly affect the strength of the immune system, which works hand in hand with the endocrine system, a hormone imbalance caused by constant fear can indeed sabotage one’s immunity. The major hormones that can have a significant impact on the immune system include steroid hormones (e.g., estrogen, testosterone, progesterone, prolactin, and glucocorticoids), oxytocin, and serotonin.
For instance, estrogen has been shown to boost women’s immune systems, as their immune systems are generally the strongest during their reproductive years when estrogen is at its highest level. As testosterone generally inhibits the immune system, it’s quite possible that women tend to have a higher prevalence of autoimmune disease than men due to the estrogen in their bodies. Autoimmune conditions can sometimes relate to hormone imbalances.
Therefore, fear can cause a hormone imbalance, which, in turn, can lead to problems with the immune system.
Fear Can Cause Other Illness
1. Fear of Symptoms Can Trigger Those Symptoms
In a study of adjuvant chemotherapy, which was published in the World Journal of Surgery, 40 participants (31 percent) of the control group, who received a placebo injection, developed alopecia. Alopecia affects approximately 65 percent of patients who receive cancer treatment. Therefore, such a high percentage of alopecia among the control group suggests that it was their fear of chemotherapy side effects that caused the hair loss to occur.
2. Fear Locks the Body Out of ‘Rest-and-Restore’ Mode
Constant fear can make the body stuck in fight-or-flight mode, which is controlled by the sympathetic nervous system of the autonomic nervous system. As a result, the body can’t enter “rest-and-restore” mode, which is controlled by the parasympathetic nervous system. This system helps the body stay in equilibrium by activating more restful functions, such as decreasing the heart rate and relaxing the muscles.
So if fear over the long term prevents the body from entering rest-and-restore mode, the body can’t relax or rest, and diseases can eventually result.
3. Fear Causes Sleep Disruption and Food Deregulation
When people are in a fearful state of mind, they tend to have poor sleep quality, which can lead to several chronic diseases and conditions.
When some people feel fearful, they want to eat sweet and fatty foods full of additives, which can cause inflammation in the body if consumed over the long term. Also, the consumption of unhealthy foods can damage the gut microbiome, and 70 percent of the immune system is located in the gut.
4. Long-Term Fear Can Cause Other Conditions
Constant fear can induce anxiety, hypochondria, high blood pressure, asthma, and depression. Since fear can affect the neuroendocrine-immune system, it also has an impact on our growth and development, as well as reproductive, urinary, and respiratory functions.
Furthermore, fear can create toxins in the brain that make it foggy and prevent it from functioning at its best. Thus the brain can’t pay attention to the body’s health as it should. For example, the fogginess might cause one to forget to take their medicine on time.
3 Ways to Mitigate the Negative Effects of Fear
Since fear has so many aforementioned negative impacts on the body, especially the immune system, we need to find ways to mitigate these effects.
1. Face Fear Head-On and Release Negative Feelings
In her book “Radical Remission: Surviving Cancer Against All Odds,” researcher and lecturer in the field of integrative oncology Kelly Turner, who holds a doctorate in social sciences research, mentioned an alternative healer’s perspective on fear. This healer is Patti Conklin, who holds a doctorate in humanities and divinity. According to Conklin, fear is a dominant emotion for most cancer patients.
According to Conklin, a patient should face fear head-on in order to release it. One example mentioned in “Radical Remission” is about a man named Nathan who was diagnosed with a rare form of stage 4 lymphoma. Unfortunately, instead of eradicating it, several rounds of chemotherapy made his cancer grow. As a result, he decided to stop the treatment, and his doctors informed him that he only had one to two years to live. He didn’t sleep for four days, fearing death.
Eventually, he decided to face his fear and accept the fact that he was going to die. To his surprise, once he made the acceptance, his fear was gone.
When he sat down to be interviewed by Turner six years later, he had been traveling, enjoying natural sceneries, and receiving help from alternative healers. He had outlived his doctors’ predictions by at least four years.
2. Replace Fear With Positive Feelings
Another effective way to deal with fear is to replace it with positive emotions, such as gratitude and happiness.
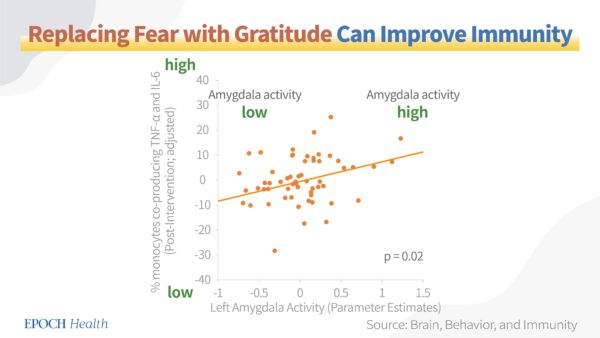
According to one study published in the journal Brain, Behavior, and Immunity, gratitude can bring health benefits in women and increases in support-giving were associated with reduced amygdala activity.
The participants in the study were asked to perform a gratitude task. After the completion of this task, those who showed larger reductions in amygdala activity also experienced larger reductions in the production of pro-inflammatory markers, including tumor necrosis factor-alpha, and interleukin-6. By replacing fear with gratitude, the immune system improved.
3. Boost Immunity
Sometimes fear is inevitable, although one may try to release or replace it with another emotion. In this case, one can focus on boosting the immune system, which can somewhat offset the negative effects brought by fear.
Ways to improve your immunity include but aren’t limited to maintaining a healthy diet with a lot of vegetables and healthy protein, being physically active and avoiding a sedentary lifestyle, keeping fit with a healthy weight, getting sufficient high-quality sleep, and quitting or avoiding smoking and alcohol consumption.